At a routine dentist appointment, my ten-year-old daughter suddenly went silent, her eyes fixed on the floor. When the visit ended, the dentist discreetly slipped me a folded note—careful that my husband didn’t see. I read it once and felt my stomach drop. I didn’t confront anyone. I didn’t ask questions out loud. I secured my daughter, documented everything, and made a few urgent calls. By the next night, the calm had shifted. Phones were ringing. Doors were closing. And my husband—the one who’d laughed it off—was the one panicking.
It was supposed to be a routine dentist appointment.
My ten-year-old daughter, Mia, sat in the chair swinging her feet while the hygienist adjusted the light. She’d been chatty on the drive over, complaining about school and asking if we could get smoothies afterward. But halfway through the visit, something changed.
She went silent.
Not sulky. Not bored. Still. Her eyes fixed on the floor, her hands clenched tightly in her lap. When the dentist, Dr. Lewis, asked a gentle question, Mia nodded without speaking.
I felt it immediately—that quiet alarm parents learn to recognize.
The appointment ended quickly after that. As we stood to leave, Dr. Lewis walked us to the front desk. My husband, Aaron, was already there, scrolling on his phone, joking about how kids always “hate the dentist.”
Dr. Lewis smiled politely. Then, as Aaron turned to answer a call, she slipped a folded note into my hand.
She did it carefully. Deliberately.
Her eyes met mine for just a second, and she said softly, “Please read this when you’re alone.”
My stomach dropped.
I didn’t open it there. I didn’t react. I thanked her, took Mia’s hand, and walked out like everything was normal. Aaron laughed about cavities. Mia stayed quiet.
In the car, after dropping Aaron at work, I parked two blocks away and unfolded the note.
It was short. Professional. Precise.
It stated that during the exam, Mia had shown physical indicators and behavioral responses that raised serious safeguarding concerns. That Dr. Lewis was mandated to report what she’d observed—but wanted me to be aware first. And that time mattered.
I read it twice.
I didn’t cry.
I didn’t scream.
I didn’t confront anyone.
I looked at my daughter in the rearview mirror and said calmly, “We’re going to go somewhere safe, okay?”
She nodded. Relief flickered across her face.
That was the moment I stopped pretending everything was fine—and started acting.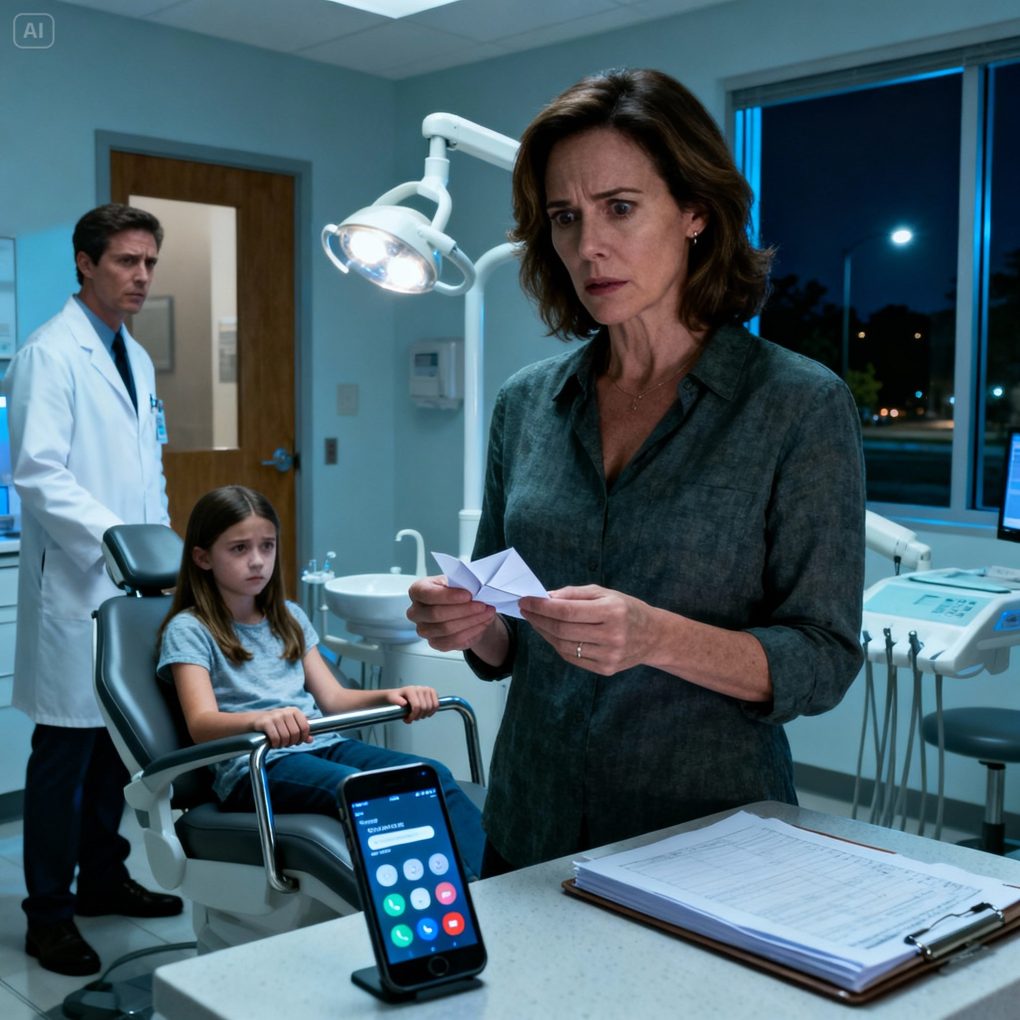
I moved fast, but not loudly.
First, I took Mia to my sister’s house. I told her we were having a sleepover. I didn’t explain more than necessary. I made sure Mia felt calm, watched, protected.
Then I started documenting.
I photographed the note. I wrote down the exact time and date. I saved appointment records. I wrote a timeline of recent changes—when Mia became withdrawn, when she stopped wanting to be alone with certain people, when she started asking to sleep with the light on.
Patterns I hadn’t wanted to see before suddenly aligned.
Next, I made calls.
Not to family.
Not to my husband.
To people whose job it is to listen when something feels wrong.
Child protection services.
A family attorney.
A child advocacy center recommended by the dentist.
Each conversation was careful. Grounded. Evidence-based. No speculation—only facts, observations, documentation.
That evening, Aaron called, annoyed.
“Why is Mia staying over there?” he asked. “You’re overreacting. Dr. Lewis always acts dramatic. You’re paranoid.”
I didn’t argue.
“I’m following professional guidance,” I said evenly.
He laughed. “This is ridiculous.”
I let him laugh.
Because by then, the report had already been filed. Appointments had been scheduled. Safeguards had been put in place.
The system was moving—quietly, deliberately.
And systems don’t care about laughter.
By the next night, the calm had shifted.
Aaron noticed first when his phone wouldn’t stop ringing.
Questions. Requests. Notifications. A meeting he needed to attend immediately. People asking about Mia—why she wasn’t home, why she’d missed school, why professionals were involved.
His tone changed.
“This is serious,” he said, suddenly tense. “Why are they calling me?”
I replied calmly, “Because concerns were raised. And they’re being addressed.”
That’s when he panicked.
He accused me of betrayal. Of exaggeration. Of destroying the family. He begged me to “fix it,” to tell them it was all a misunderstanding.
“I can’t undo facts,” I said. “And I won’t silence my child to make things comfortable.”
Mia was interviewed gently by trained professionals. She wasn’t pressured. She wasn’t rushed. For the first time in weeks, she slept through the night.
Dr. Lewis followed protocol. Others did too.
Doors closed—not with drama, but with procedure. Access changed. Supervision rules were enforced. The world Aaron assumed would protect him by default… didn’t.
He kept saying, “I didn’t think it was real.”
That sentence told me everything.
This story isn’t about blame or revenge.
It’s about believing children the first time they go quiet.
About listening when professionals act carefully instead of loudly.
About choosing protection over denial—even when denial would be easier.
If this story stayed with you, consider this:
Do you trust your instincts when something feels wrong, even if others dismiss it?
And are you prepared to act quietly—but decisively—when a child’s safety is at stake?
Sometimes the bravest thing a parent can do isn’t confrontation.
It’s documentation, action, and refusing to let anyone laugh away a warning that was never meant to be ignored.

