My ten-year-old’s surgery failed, leaving him unresponsive. My husband said mistakes happened and told me to move on. I couldn’t.
Late that night, a young resident slipped into the room, eyes darting to the door. He lowered his voice and told me to check the surgical records. His hands were shaking.
“The surgeon wasn’t authorized to perform that procedure,” he whispered.
I felt the room spin.
Because suddenly, my son’s condition wasn’t a tragedy anymore.
It was evidence.
The surgery was supposed to be routine.
That was the word they used over and over—routine—as if repeating it enough times could make it true. My son, Ethan, was ten years old, small for his age, nervous but brave. He squeezed my hand before they wheeled him away and asked if I’d be there when he woke up.
“I promise,” I said.
The hours dragged. When the surgeon finally came out, his expression was too controlled, too neutral. He spoke carefully, choosing words like complication and unexpected outcome. Ethan wasn’t waking up. They were monitoring him. We needed to be patient.
By nightfall, he was still unresponsive.
Machines breathed for him. Lines ran into his arms. His face looked peaceful in a way that felt wrong, like stillness pretending to be rest.
My husband stood beside me, arms folded, jaw tight. “Mistakes happen,” he said quietly, already exhausted by the day. “The doctors did what they could. We can’t live in this room forever.”
I stared at our son and felt something harden inside my chest.
“I’m not moving on,” I said.
He sighed, frustrated, and left to get coffee. The room settled into the low hum of monitors and the soft shuffle of nurses’ shoes outside the door.
It was close to midnight when the door opened again.
A young resident stepped in, barely older than a student. He hesitated, then closed the door behind him. His eyes flicked toward the hallway, then back to me. His hands were shaking.
“I shouldn’t be here,” he whispered.
My heart began to race.
“There’s something you need to look at,” he said, lowering his voice further. “The surgical records. Please.”
I stood slowly. “What are you saying?”
He swallowed. “The surgeon wasn’t authorized to perform that procedure.”
The room tilted.
Because suddenly, my son’s condition wasn’t a tragedy anymore.
It was evidence.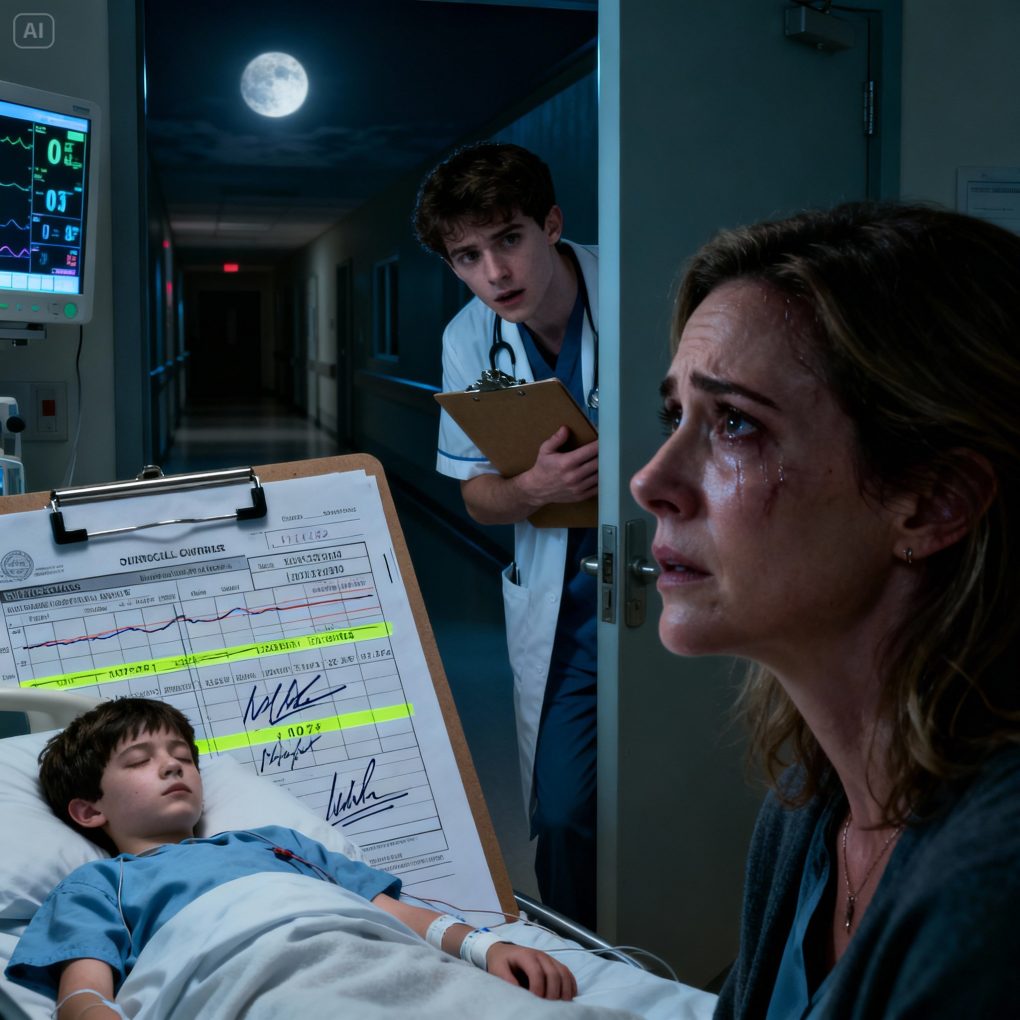
I didn’t sleep that night.
After the resident left, I sat beside Ethan’s bed, replaying his words until they felt carved into my bones. Not authorized. Not a mistake. Not bad luck.
By morning, I requested the records.
At first, the staff hesitated. Policies. Procedures. Waiting periods. I didn’t argue. I just stayed there, calm and unmoving, until a patient advocate arrived.
When the documents finally came, the truth wasn’t hidden—it was buried under assumptions no one expected a grieving mother to question.
The surgeon who operated on my son was licensed, respected, experienced. But that specific procedure required additional certification. He didn’t have it. He’d been denied approval months earlier due to insufficient training hours.
Someone had signed off anyway.
The resident’s note wasn’t in the file. Neither was a required consult. Timelines didn’t match. Pages were missing.
I asked my husband to look with me. He glanced at the papers, then pushed them back gently. “This won’t change anything,” he said. “You’re going to destroy yourself chasing this.”
I realized then that we were standing in two different realities.
For him, acceptance was survival.
For me, silence felt like betrayal.
That afternoon, hospital administrators requested a meeting. Their voices were careful, sympathetic, heavy with rehearsed concern. They said an internal review was underway. They said outcomes like this were rare but unavoidable.
I asked one question.
“Why was an unauthorized surgeon allowed into that operating room?”
No one answered right away.
That was enough.
By evening, an external investigation was opened. The resident came forward officially. Others followed—nurses, technicians, staff who had felt something was wrong but didn’t think anyone would listen.
Ethan remained unresponsive.
But the story around him was finally waking up.
The findings took weeks.
During that time, my son lay in the same bed, his future uncertain, his body bearing the weight of someone else’s decision. I learned how systems protect themselves first. How quickly concern turns into containment.
The surgeon was suspended. Then terminated. The hospital admitted fault—not loudly, not publicly at first, but clearly enough to matter. Lawsuits followed. Policies changed. Oversight tightened.
My husband apologized eventually. Not for doubting me, but for wanting the pain to end more than he wanted the truth.
I understood that. But I didn’t share it.
Ethan opened his eyes one morning without warning. Not fully aware. Not healed. But present. And that was enough to keep going.
What stays with me isn’t the anger, or even the grief. It’s how close the truth came to disappearing under words like accident and acceptance.
If that resident hadn’t been brave enough to speak, my son’s story would have ended as a statistic. A sad outcome. A closed file.
Instead, it became a record.
Evidence doesn’t heal wounds. But it does something just as important—it refuses to let harm be dismissed as fate.
If you’ve ever felt pressured to “move on” when something inside you said the story wasn’t finished, trust that voice.
Sometimes the difference between tragedy and justice is one person who refuses to look away.



